ESI $60 Million Verdict
The Baltimore Medical Malpractice Lawyer Blog reports medical malpractice verdicts. This report highlights a verdict for ESI medical malpractice.
Understanding the Risks of Epidural Steroid Injections: A Case Study in Spinal Cord Infarction
A jury awarded over $60 million to a man after a routine epidural steroid injection (ESI) permanently paralyzed him. The procedure allegedly resulted in a spinal cord infarction. This case highlights the extremely bad outcomes that can arise from this common medical procedure. It also stresses the importance of proper technique and steroid selection.
What is an Epidural Steroid Injection?
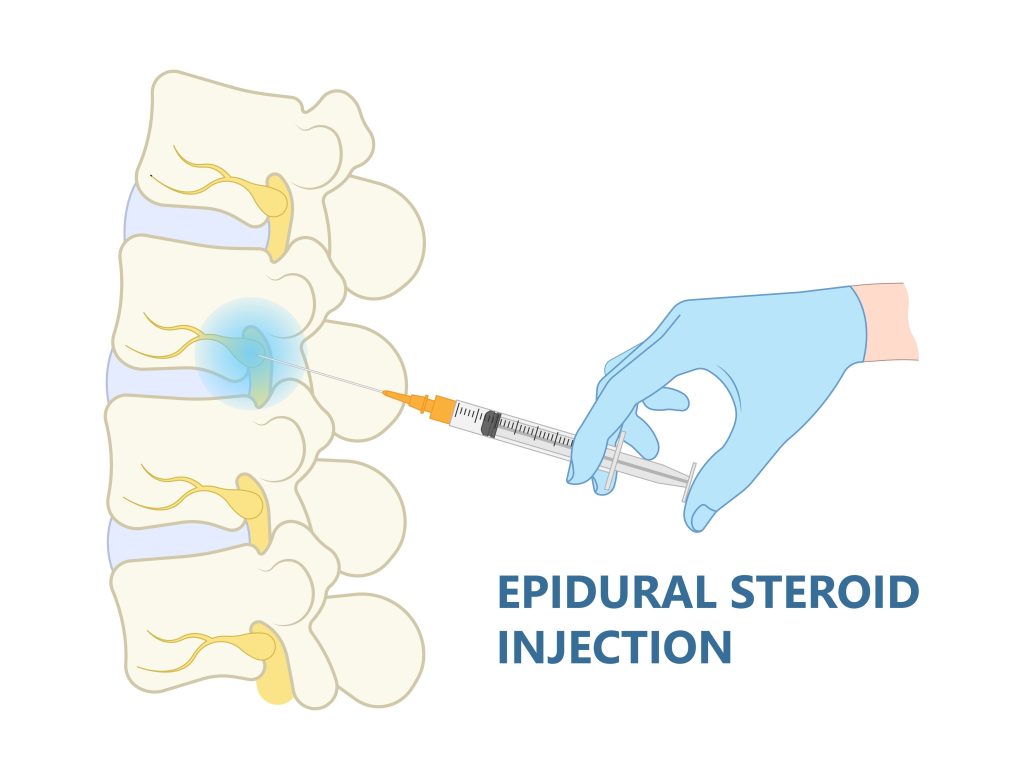
An epidural steroid injection is a procedure in which anti-inflammatory medicine, such as a steroid or corticosteroid, is injected into the epidural space of the spine. The epidural space is the area surrounding your spinal nerves. This treatment commonly manages pain caused by irritation and inflammation of the spinal nerve roots, often associated with conditions like spinal stenosis or a herniated disc. The medication is a combination of a corticosteroid and a local anesthetic.
A Brief History of Epidural Steroid Injections
The concept of epidural injections for pain management dates back to the early 1900s. The first record of use was around 1901 by French physicians Jean-Athanase Sicard and Fernand Cathelin, who injected cocaine through the sacral hiatus to treat conditions like sciatica. Over time, the technique also began to use local anesthetics. In the early 1950s, corticosteroids started in epidural use. Since the 1970s, numerous clinical trials have shown that ESIs can have a significant, though small, short-term effect on leg pain. Despite ongoing debate about their effectiveness and safety, ESIs are now one of the most widely utilized pain management procedures in the world.
Technique and the Critical Role of Imaging
Proper administration of an ESI is crucial to minimizing risk and avoiding medical malpractice. The doctor can perform the procedure using an interlaminar approach, where he places the needle between the vertebral lamina, or a transforaminal approach, where the doctor places the needle into the neural foramen next to the exiting nerve root.
Image guidance is essential for the accurate placement of the needle and the safe delivery of the medication. Doctors use imaging techniques like computed tomography (CT) or X-ray fluoroscopy to guide in real-time. A contrast medium or air is often injected to confirm the needle’s position in the epidural space before the steroid is administered. This step helps to ensure that doctor does not accidentally inject the medication into a blood vessel or the intrathecal space (the fluid-filled area surrounding the spinal cord), which can lead to serious complications.
The Steroid Choice: Particulate vs. Non-Particulate
The type of corticosteroid used in an ESI is a key factor in the safety of the procedure, as highlighted in the Gangaram case. Steroids are classified as either particulate or non-particulate. Particulate preparations, such as methylprednisolone acetate (Depo-Medrol), triamcinolone acetonide (Kenalog), and betamethasone acetate, contain undissolved crystals. These crystals are often large enough to occlude the small arteries that supply the spinal cord. Non-particulate preparations, like dexamethasone, dissolve completely and do not contain these crystals.
The use of particulate corticosteroids, particularly in the cervical spine, can have catastrophic complications, including paralysis and even death. The theoretical benefit of particulate steroids is that their anti-inflammatory effect is delayed but sustained because the crystals are released gradually. However, non-particulate preparations are safer due to the lack of risk of embolic events. This case specifically noted the use of Kenalog, a particulate steroid, which plaintiffs argued was a contributing factor to his injury.
What Can Go Wrong? ESI Medical Malpractice
While generally considered a safe procedure, ESIs carry potential risks and bad outcomes. Minor side effects can include a “steroid flush,” increased blood sugar, and pain at the injection site. More serious, though rare, bad outcomes can include:
- Infection: Infections can range from meningitis to epidural abscesses and are often due to poor sterile technique.
- Bleeding/Hematoma: A collection of blood at the injection site can occur.
- Nerve Damage: Direct trauma to a nerve or the spinal cord itself is a possibility.
- Intravascular Injection: This is one of the most serious risks, where the doctor accidentally injects medication into a blood vessel. The FDA has issued a warning that this can lead to serious events like loss of vision, stroke, paralysis, and death.
- Spinal Headache: A severe headache can result if cerebrospinal fluid leaks out of the epidural region.
- Spinal Cord Infarction: This is the most severe and rare bad outcome, as seen in the this case.
Spinal Cord Infarction: The Ultimate Risk of ESI Medical Malpractice
A spinal cord infarction is a stroke that occurs within the spinal cord. It is caused by a blockage of the blood supply to the spinal cord, leading to the death of nerve tissue. Symptoms often appear suddenly and can include sharp back pain, weakness, and paralysis in the legs or arms.
The mechanism by which an ESI can cause a spinal cord infarction is most often inadvertent intra-arterial injection, particularly with particulate steroids. A needle, especially during a transforaminal injection, can accidentally enter a radicular artery that supplies the spinal cord. If a doctor injects a particulate steroid into this artery, the tiny crystals can travel. They can cause a blockage (embolism) in the smaller, more distal arteries of the spinal cord. This can cut off the blood supply to a section of the spinal cord, resulting in an infarction. This case of illustrates this risk, with experts stating that the use of a particulate steroid and wrong technique led to his permanent paraplegia. This tragic outcome is a powerful reminder of the potential for severe, life-altering complications, even in what is a routine medical procedure.
Next Step: Call Baltimore ESI Medical Malpractice Lawyer Mark Kopec
If you have been injured by ESI medical malpractice, call Baltimore ESI Lawyer Mark Kopec now.
Mark Kopec is a top-rated Baltimore medical malpractice lawyer. Contact us at 800-604-0704 to speak directly with Attorney Kopec in a free consultation. The Kopec Law Firm is in Baltimore and helps clients throughout Maryland and Washington, D.C. Thank you for reading the Baltimore Medical Malpractice Lawyer Blog.





