Placenta Percreta $17M
Parties reached a $17 million settlement in a placenta percreta birth injury case. This marked a significant moment for medical malpractice and obstetric care. The case involved a mother who filed a lawsuit against her doctor, an OB/GYN and maternal fetal medicine doctor, and a hospital. This followed a harrowing experience that left her daughter with lifelong injuries.
The lawsuit alleged medical negligence in the timing of a C-section for a high-risk pregnancy. This then led to a uterine rupture and subsequent oxygen deprivation for the newborn. While the defense maintained their approach met medical standards, the settlement underscores the critical nature of managing complex placental conditions.
Anatomy of the Placenta: The Life Support System
The placenta is a vital, temporary organ that forms in the uterus during pregnancy. It acts as the primary communication link between the mother and the developing fetus, responsible for providing oxygen and nutrients while removing waste products via the umbilical cord.
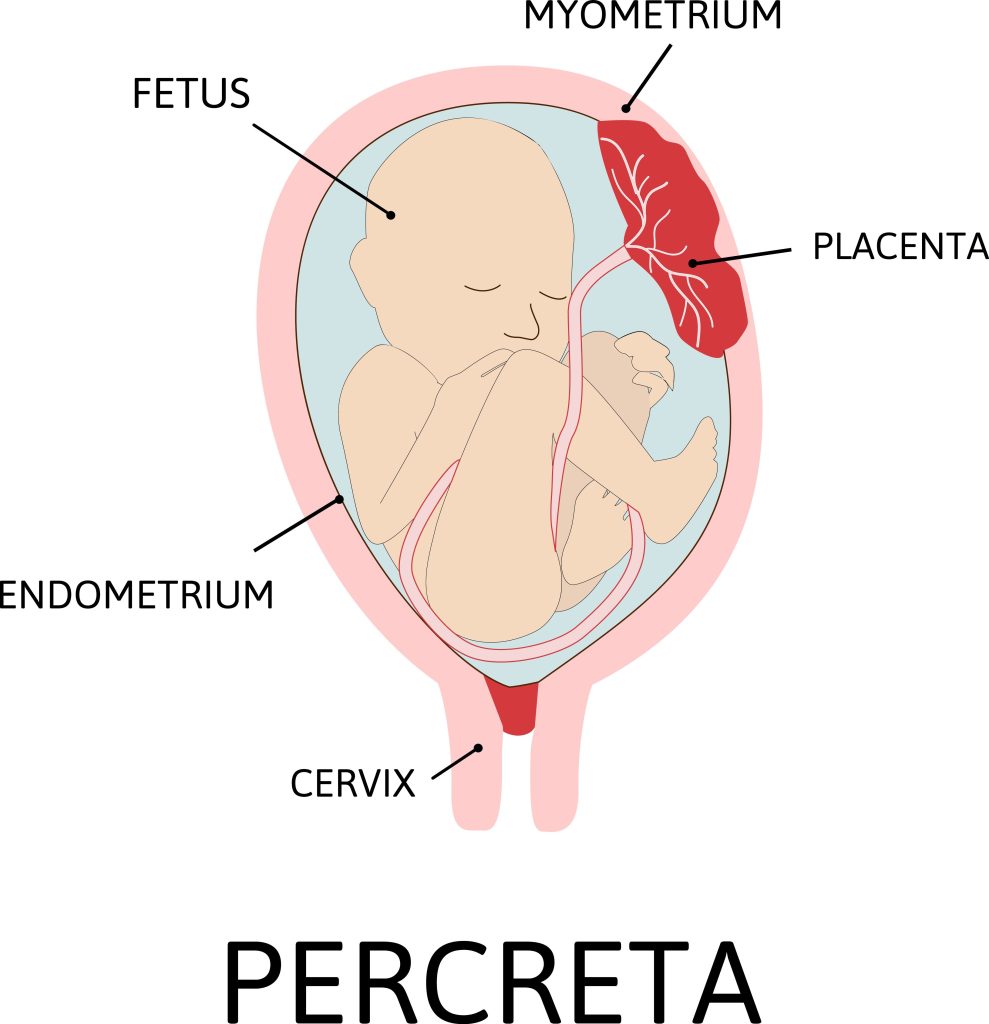
Structurally, the placenta consists of both fetal and maternal components. The fetal side, known as the chorion, develops branching structures called chorionic villi. These villi are essential for nutrient exchange as they dip into the mother’s blood supply within the uterine wall. Normally, these villi attach to the endometrium (the inner lining of the uterus) and detach easily after birth.
Understanding Placenta Percreta Birth Injury: When Invasion Becomes Dangerous
Placenta percreta is specifically the most severe form of “placenta accreta spectrum” (PAS), a range of conditions where the placenta attaches too deeply to the uterine wall.
- Placenta Accreta: The villi attach to the superficial muscle of the uterus.
- Placenta Increta: The villi grow deeper into the uterine muscle (myometrium).
- Placenta Percreta: The most catastrophic type, where the placenta grows entirely through the uterine wall and may invade nearby organs like the bladder or intestines.
In this case, her diagnosis of placenta percreta meant that the placental tissue breached the outer uterine layer and severely compromised the structural integrity of her uterus.
Causes and Risk Factors of Placenta Percreta Birth Injury
The leading theory is that a “defective” decidua (uterine lining) allows for uncontrolled placental invasion. This often occurs at the site of previous surgical scars.
The primary risk factors include:
- Previous Cesarean Sections: This is the single most important risk factor; the more C-sections a woman has had, the higher the risk.
- Placenta Previa: A condition where the placenta covers the cervix.
- Uterine Surgery: History of fibroid removal (myomectomy) or dilation and curettage (D&C).
- Advanced Maternal Age: Typically defined as age 35 or older.
Diagnosis: Who and How?
Suspected cases of PAS are typically managed and diagnosed by Maternal-Fetal Medicine (MFM) specialists—doctors who specialize in high-risk pregnancies.
The primary diagnostic tools are:
- Prenatal Ultrasound: Often performed during the second-trimester anatomy scan, it has a sensitivity of over 90% for detecting placental abnormalities.
- MRI: Used as an adjunct to ultrasound, MRI provides better detail of the depth of invasion and whether the placenta has reached the bladder or other pelvic organs.
Baltimore birth injury lawyer Mark Kopec can assess the diagnosis of your placenta percreta and advise you on a potential birth injury case.
The Treatment Plan: Management of a High-Risk Delivery
Because of the extreme risk of life-threatening hemorrhage, a “C-hysterectomy” (delivering the baby via C-section followed immediately by the removal of the uterus) is the standard of care.
The delivery is typically scheduled prematurely, often between 34 and 37 weeks, to avoid the mother going into spontaneous labor, which could trigger a rupture. In this case, she was scheduled for 37 weeks, but the lawsuit argued this delay was negligent as her uterus ruptured before the procedure could take place.
Uterine Rupture: A Catastrophic Event
A uterine rupture is a full-thickness tear of the uterine wall. In placenta percreta, the invading placental villi weaken the uterine muscle to the point of failure. As the pregnancy progresses and the uterus stretches, the thinned, invaded section can then spontaneously burst.
Placenta Percreta Birth Injuries: HIE and Cerebral Palsy
When a uterus ruptures, it is a medical emergency for both mother and child. For the baby, the rupture often disrupts the blood and oxygen supply from the placenta.
- HIE: Hypoxic Ischemic Encephalopathy: This is a brain injury caused by a lack of oxygen (hypoxia) and a lack of blood flow (ischemia). If the brain is deprived of oxygen for even a few minutes, brain cells begin to die.
- Cerebral Palsy (CP): HIE is a leading cause of cerebral palsy, a permanent neurological disorder that affects motor skills, muscle tone, and also movement.
In this case, the uterine rupture led to baby to suffer from HIE. This ultimately resulted in her developing cerebral palsy. This $17 million settlement will provide for the baby’s lifetime medical needs, including specialized therapies and accommodations required for her condition.
You can read Blog posts on other delayed c-section cases:
- Pitocin Misuse $951M
- Prolonged Labor $48 Million
- Fetal Decelerations $29M
- Preeclampsia Stillbirth $25M
- Delayed C-Section $18M
Mark Kopec is a top-rated Baltimore medical malpractice lawyer. Contact us at 800-604-0704 to speak directly with Attorney Kopec in a free consultation. The Kopec Law Firm is in Baltimore and helps clients throughout Maryland and Washington, D.C. Thank you for reading the Baltimore Medical Malpractice Lawyer Blog.





