Mark Kopec Now
Optic Nerve
🩺 Medical Malpractice and the Optic Nerve: A Pathway to Permanent Blindness
The optic nerve is a seemingly small structure. However, it is the critical “cable” that transmits all visual information from the eye to the brain. Consequently, damage to this nerve, which carries over a million nerve fibers, can lead to severe and often permanent vision loss or total blindness. When such devastating injury to the optic nerves occurs as a result of a healthcare provider’s negligence, it forms the basis of a medical malpractice claim.
The Anatomy and Function of the Optic Nerve
The optic nerve is not a peripheral nerve. It is technically part of the central nervous system (CNS). This means its ability to regenerate after injury is extremely limited. Accordingly, it leads to irreversible vision loss.
Anatomy: Cranial Nerve II (CN II)
- Formation: The nerve fibers exit the eye through a mesh-like structure called the lamina cribrosa. This point is devoid of photoreceptors, creating a natural blind spot.
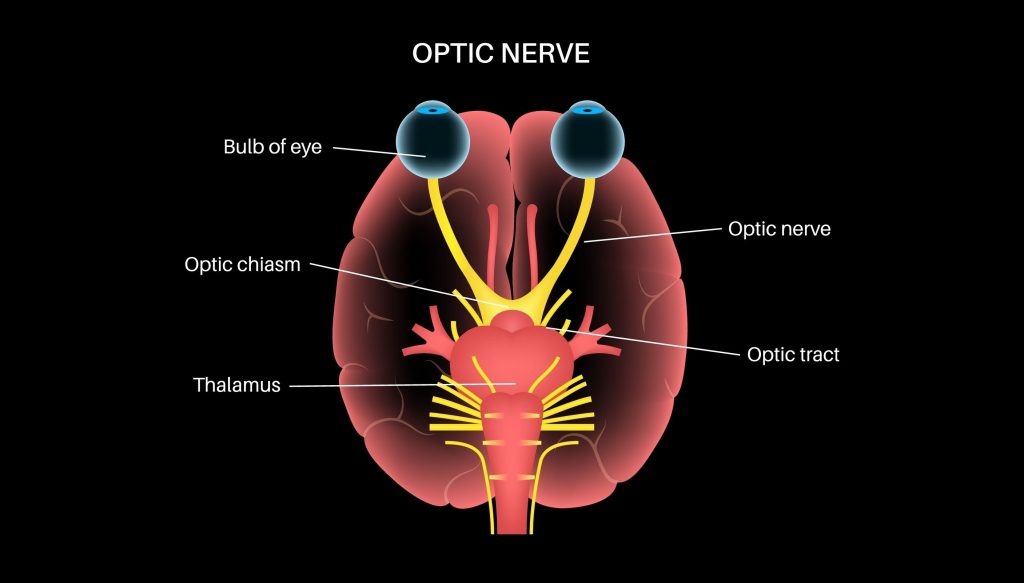
- Course: It then travels through the orbit (eye socket) and a bony canal (optic canal) into the skull.
- The Optic Chiasm: Within the brain, the two optic nerves meet at the optic chiasm. At this X-shaped junction, fibers from the nasal (inner) half of each retina cross over to the opposite side of the brain, while fibers from the temporal (outer) half stay on the same side. This crossing is essential for binocular vision and depth perception.
- The Optic Tracts: After the chiasm, the fibers continue as the optic tracts to relay stations in the brain, primarily the lateral geniculate nucleus (LGN) of the thalamus, before reaching the visual cortex in the occipital lobe, where the image is processed.
Function: Translating Light to Sight
The primary function of the optic nerve is purely sensory: to relay the electrical impulses created by the light-sensitive retina to the brain. Without the optic nerve, the eye cannot translate light detection into conscious sight.
It also plays a crucial role in two important reflexes:
- Pupillary Light Reflex: The optic nerve is the afferent (input) limb that signals the brain about the intensity of light, prompting the oculomotor nerve (CN III) to constrict or dilate the pupils to regulate light entry.
- Accommodation Reflex: It is also the input for the reflex that adjusts the lens shape to allow the eye to focus on near objects.
🔪 Ways the Optic Nerve is Injured by Medical Malpractice
Optic nerve damage in a medical malpractice context typically falls into three main categories: Failure to Diagnose/Treat, Surgical Error, and Anesthesia/Perioperative Mismanagement. Given the optic nerve’s central nervous system classification, most resulting vision loss is irreversible.
1. Misdiagnosis or Failure to Diagnose and Treat Glaucoma
Medical Condition/Treatment: Glaucoma is a group of eye conditions that damage the optic nerve, often due to abnormally high pressure in the eye (intraocular pressure, or IOP). Early diagnosis and treatment are critical to managing IOP and preventing progressive, irreversible nerve damage.
Medical Providers Involved: Ophthalmologists, Optometrists, and sometimes general practitioners or emergency department physicians who fail to refer a patient promptly.
How the Optic Nerve is Injured: The negligence occurs when a provider fails to perform standard diagnostic tests (like tonometry to measure IOP, or a visual field test), or fails to correctly interpret the results. This leads to a delayed diagnosis or misdiagnosis. The high IOP continuously compresses and damages the delicate axons of the optic nerve over time. This is a process that the doctor could slowed or halted with medication or surgery.
Prognosis: The prognosis is poor for vision already lost, as this damage is generally irreversible. The malpractice claim would focus on the extent of vision loss (peripheral vision loss, central vision loss, or total blindness) that occurred during the period of negligent delay.
2. Ischemic Optic Neuropathy (ION) due to Perioperative Negligence
Medical Condition/Treatment: Post-operative vision loss (POVL) following non-ocular surgery. This includes extensive spine, cardiac, orthopedic, or head and neck procedures, particularly those involving prone positioning (face down) or prolonged surgery. The injury is Ischemic Optic Neuropathy (ION), which is damage to the optic nerve due to a lack of sufficient blood flow (ischemia) and oxygen.
Medical Providers Involved: Anesthesiologists, Certified Registered Nurse Anesthetists (CRNAs), and Surgeons.
How the Optic Nerve is Injured: Malpractice in this context centers on the failure to adequately monitor the patient’s hemodynamics (blood pressure and blood flow) and/or improper positioning during prolonged general anesthesia.
- Hypotension: Negligently allowing the patient’s blood pressure to drop too low (hypotension) for too long. This reduces blood flow to the optic nerve, causing oxygen starvation and cell death.
- Prone Positioning: In spine surgery, the doctor often places a patient face-down. Improper head positioning or excessive pressure on the eyes can directly impede the blood supply via the ophthalmic artery or increase venous pressure. This can lead to ischemia.
Prognosis: ION resulting in POVL is a catastrophic event, and the resulting vision loss (which can range from partial to total blindness in one or both eyes) is often permanent and severe.
3. Direct Mechanical or Thermal Injury during Surgery
Medical Condition/Treatment: Surgical procedures performed in close proximity to the optic nerve. This includes ophthalmic surgeries (e.g., complicated retinal detachment repair, glaucoma surgery), nasal/sinus surgeries (due to the nerve’s proximity to the sinuses), and neurosurgery (e.g., tumor removal near the optic chiasm, like a pituitary tumor).
Medical Providers Involved: Ophthalmologists (Retina Specialists, Glaucoma Specialists), Otolaryngologists (ENT surgeons), and Neurosurgeons.
How the Optic Nerve is Injured: The injury is typically a direct surgical error involving the negligent use of instruments:
- Transection/Tearing: Inadvertently cutting or tearing the optic nerve or surrounding blood vessels with a scalpel, drill, or other surgical tool.
- Thermal Damage: Using a laser or electrocautery device improperly, leading to burn damage of the nerve fibers.
- Pressure/Hematoma: Post-operative bleeding (hematoma) or excessive swelling that the doctor does not manage immediately. This can create pressure (orbital compartment syndrome) that compresses the nerve and cuts off its blood supply. The malpractice is often the failure to recognize and immediately treat the compartment syndrome.
Prognosis: Direct trauma is usually immediate and devastating. The loss of sight is often profound and permanent, as central nervous system tissue has extremely limited capacity for regeneration. If intervention is immediate (e.g., relieving pressure from a hematoma), the prognosis may be slightly better, but delays are catastrophic.
Seeking Justice for Medical Malpractice After Optic Nerve Damage
For victims, the sudden and permanent loss of vision is a life-altering tragedy. In a medical malpractice case involving optic nerve damage, the plaintiff must prove that the medical provider’s care fell below the accepted standard of care. In addition, this negligence was the direct cause of the irreversible vision loss. No legal action can restore sight. However, a successful claim can provide the necessary compensation for lifelong care. This can include adaptive technologies, lost wages, and pain and suffering related to the trauma of blindness.
If you have a permanent optic nerve injury, see below to contact the Kopec Law Firm.
Visit our free consultation page or video. Then contact the Kopec Law Firm at 800-604-0704 to speak directly with Attorney Mark Kopec. He is a top-rated Baltimore medical malpractice lawyer. The Kopec Law Firm is in Baltimore and pursues cases throughout Maryland and Washington, D.C.





