Mark Kopec Now
Pap Smear
The Lifeline of Cervical Health: Understanding Pap Smears and Medical Malpractice
The Papanicolaou test, commonly known as the Pap smear, is one of the most successful public health interventions in medical history. Since its widespread adoption, it has reduced cervical cancer deaths by more than 70%. However, because the pap smear test relies heavily on human interpretation and strict clinical follow-up, it is also a frequent subject of medical malpractice litigation. When a doctor misreads a pap smear or poorly manages a result, the consequences are often catastrophic, allowing a highly preventable cancer to progress to advanced stages.
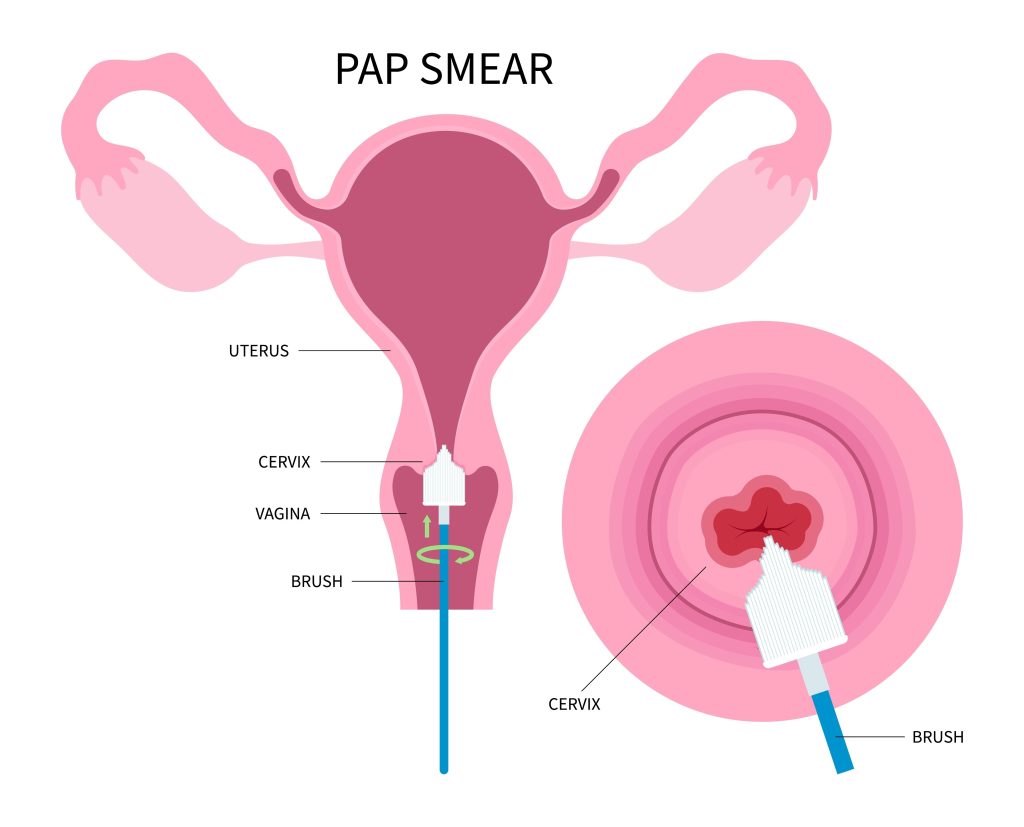
Anatomy of the Cervix: The Gateway
To understand the Pap smear, one must understand the cervix. The cervix is the lower, narrow portion of the uterus that opens into the vagina. It acts as a gateway, allowing menstrual blood to exit and sperm to enter.
The cervix has two main types of cells:
- Squamous cells: Flat, thin cells that cover the outer surface of the cervix (ectocervix).
- Glandular cells: Column-shaped cells that line the inner cervical canal (endocervix).
The area where these two cell types meet is the transformation zone. This is the most critical area for a Pap smear because it is where nearly all cervical cancers and precancerous changes begin.
A Brief History: Dr. Papanicolaou’s Discovery
The test is named after Dr. George Papanicolaou, a Greek physician who began researching vaginal cytology in the 1920s. Initially, his work was met with skepticism; the prevailing medical thought was that cancer could only be diagnosed through a tissue biopsy, not by looking at “sloughed-off” cells.
It wasn’t until 1941, when Papanicolaou published Diagnosis of Uterine Cancer by the Vaginal Smear, that the medical community realized they had a non-invasive way to detect cancer before a tumor was even visible. By the 1950s, the Pap smear became a routine part of gynecological care, transforming cervical cancer from a leading cause of death for women into a preventable condition.
How the Test Works
A Pap smear is a cytology test, meaning it examines individual cells rather than a chunk of tissue.
- The Procedure: During a pelvic exam, a provider uses a speculum to visualize the cervix. They then use a small brush or spatula to gently scrape cells from the transformation zone.
- The Processing: In the past, providers smeared these cells directly onto a glass slide (a “Conventional Pap”). Today, most providers use Liquid-Based Cytology (LBC), where the brush is rinsed into a vial of preservative liquid. This allows for a cleaner sample, as it filters out blood and mucus that might obscure the cells.
- The Interpretation: The sample is sent to a laboratory where a cytotechnologist or pathologist examines the cells under a microscope to look for abnormalities in the cell size, shape, or nucleus.
What the Pap Smear Can and Cannot Show
It is a common misconception that a Pap smear tests for “everything” related to reproductive health.
What it Can Show:
- Precancerous changes: Known as dysplasia or Cervical Intraepithelial Neoplasia (CIN).
- Early-stage cervical cancer.
- Inflammation or certain infections: Sometimes pap smears note yeast infections or trichomoniasis, though this is not the primary purpose.
- HPV presence: While not technically part of the “smear” itself, the same liquid sample is often used for co-testing to detect High-Risk Human Papillomavirus (HPV) DNA.
What it Cannot Show:
- Ovarian Cancer or Uterine Cancer: While rare “drop down” cells are sometimes caught, the Pap smear is not a reliable screening tool for these cancers.
- STIs: It does not routinely screen for Chlamydia, Gonorrhea, or Syphilis unless a doctor specifically orders additional tests.
- Infallibility: The Pap smear is a screening tool, not a diagnostic one. It has a known “false negative” rate. This is why regular, repeat screening is essential.
The Providers Involved
Several doctors and other medical providers form the “chain of care” for a Pap smear:
- Collecting Providers: Usually a Gynecologist (OB/GYN), Primary Care Physician (PCP), Physician Assistant (PA), or Nurse Practitioner (NP).
- Cytotechnologists: Laboratory professionals who perform the initial screening of the slides. They filter out the “normal” slides and flag suspicious ones.
- Pathologists: Medical doctors who specialize in diagnosing disease. They must review any slide flagged by a cytotechnologist as abnormal.
Medical Malpractice in Pap Smears
Medical malpractice occurs when a provider deviates from the standard of care, resulting in injury or death. In the context of Pap smears, claims generally fall into three categories:
1. Laboratory Errors (Misinterpretation or Misdiagnosis)
This is the most common form of Pap smear litigation. It involves a cytotechnologist or pathologist looking at a slide containing clearly abnormal cells and marking it as “Normal.”
- The Legal Standard: The law recognizes that humans make mistakes. For a misread to be “malpractice,” it must be shown that a reasonably competent professional, looking at the same slide, should have identified the abnormality.
2. Clinical Failure to Follow Up
Even if the lab correctly identifies a precancerous lesion, malpractice can occur if the doctor’s office fails to act.
- Failure to notify: The lab sends the “Abnormal” report, but the doctor’s office never calls the patient.
- Failure to refer: The doctor sees the abnormal result but fails to order a colposcopy (a more detailed exam) or biopsy.
- Administrative errors: Medical providers file results into a chart without a clinician reviewing them.
3. Failure to Screen
If a patient presents for an annual exam and the provider fails to offer or perform a Pap smear according to established guidelines (such as those from ACOG or the ACS), and the patient later develops cervical cancer, the provider may be liable.
Conclusion on Pap Smear & Medical Malpractice
The Pap smear remains a miracle of modern medicine, but its success depends on a flawless handoff of information between the patient, the clinician, and the lab. When a link in that chain breaks, a patient loses the opportunity for early intervention—turning a treatable condition into a life-threatening one.
If you suspect a delay in diagnosis occurred despite regular screening, it is vital to have the original pathology slides reviewed by an independent expert.
If you have any concerns or questions about pap smear medical malpractice, then visit the Kopec Law Firm free consultation page or video. Then contact us at 800-604-0704 to speak directly with Attorney Mark Kopec. He is a top-rated Baltimore medical malpractice lawyer. The Kopec Law Firm is in Baltimore and pursues cases throughout Maryland and Washington, D.C.





