Mark Kopec Now
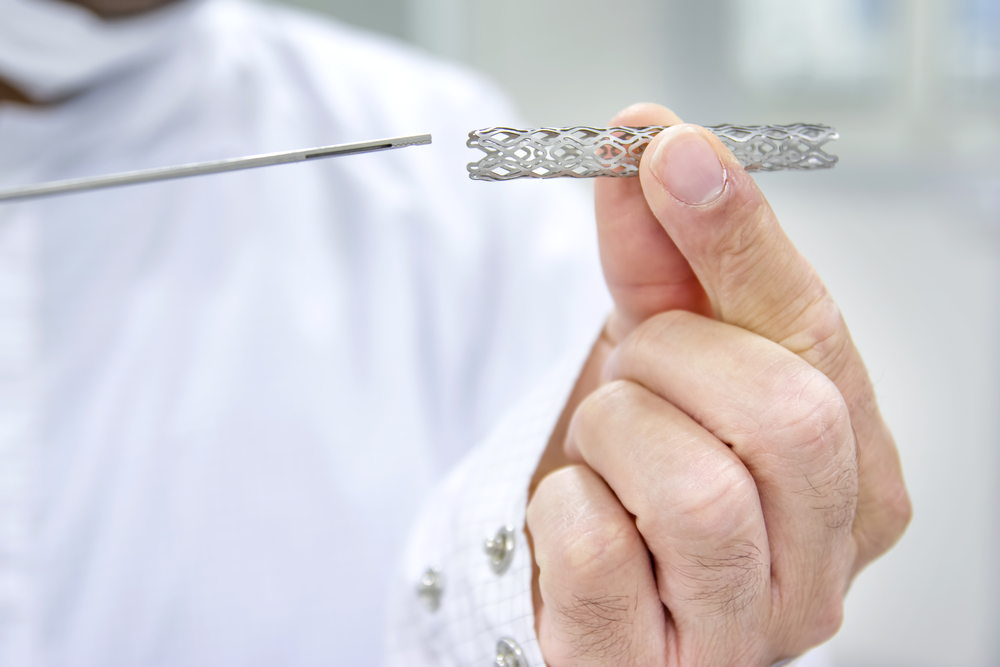
Stent
💔 Stent Medical Malpractice: Diagnosis, Placement, and Negligence
A stent is a small, mesh-like tube used to open and maintain the patency of blocked or narrowed tubular structures within the body, most commonly blood vessels (coronary or peripheral arteries) but also bile ducts, ureters, or the esophagus. While stents are life-saving devices, their necessity, selection, and placement require the utmost precision and following of the medical standard of care. Negligence at any stage—from diagnosis to placement—can form the basis of a medical malpractice claim with a stent.
📜 A Brief History of Stents
The concept of stenting has roots in the work of English surgeon Charles Stent in the middle of the 19th century, who developed a compound for dental impressions; his name was later applied to a similar concept of supporting tissue, though he did not create the device as we know it today.
The modern era of stenting began with the development of balloon angioplasty by Andreas Grüntzig in 1977. However, angioplasty alone suffered from a high rate of restenosis (re-narrowing). The solution came in the form of the first functional intravascular stent, developed by Dr. Ulrich Sigwart and successfully placed in 1986. This was the bare metal stent (BMS). The subsequent development of the drug-eluting stent (DES) in the early 2000s, which releases medication to prevent tissue overgrowth, revolutionized interventional cardiology and significantly reduced restenosis rates.
🛠️ Types of Stents and Clinical Applications
While stents are used in numerous areas of the body, the most critical malpractice risk areas involve cardiac (coronary) and vascular stenting, as well as gastrointestinal (GI) and genitourinary (GU) stenting.
1. Coronary Stents (Cardiac)
These are used to treat coronary artery disease (CAD), which generally involves plaque buildup in the heart’s arteries.
| Feature | Details |
| Symptoms/Conditions | Myocardial Infarction (Heart Attack), Angina (Chest Pain), severe blockage (70% or more) of a coronary artery. |
| Referral Providers | Cardiologists (general or non-invasive), Emergency Physicians |
| Placing Providers | Interventional Cardiologists. |
| Function | Mechanically opens a narrowed coronary artery to restore blood flow (revascularization) and reduce the risk of a heart attack. |
| Permanence | Permanent. They become embedded in the artery wall. (Some newer, rare types are bioresorbable, but most are permanent.) |
| Types | Bare Metal Stents (BMS) and Drug-Eluting Stents (DES). |
The Kopec Law Firm can assess your coronary stent history and advise you on a medical malpractice claim.
2. Peripheral Vascular Stents (Non-Cardiac Arteries)
These are used to treat Peripheral Artery Disease (PAD), where arteries supplying the limbs (especially legs) or organs like the kidneys are blocked.
| Feature | Details |
| Symptoms/Conditions | Claudication (pain upon walking), Critical Limb Ischemia (CLI), severe blockages in carotid, renal, or leg arteries. |
| Referral Providers | Vascular Surgeons, Interventional Radiologists, Cardiologists. |
| Placing Providers | Interventional Radiologists, Vascular Surgeons, Interventional Cardiologists. |
| Function | Restores blood flow to the limbs or organs to prevent tissue death, gangrene, or stroke. |
| Permanence | Permanent. |
| Types | Both BMS and DES, often larger and more flexible than coronary stents. |
Baltimore medical malpractice lawyer Mark Kopec will give you advice about peripheral vascular stents.
3. Esophageal/Biliary/GI Stents
These are used to relieve blockages in the digestive and biliary tracts.
| Feature | Details |
| Symptoms/Conditions | Malignant strictures (e.g., pancreatic cancer blocking the bile duct), Benign strictures, Esophageal tears or blockages causing dysphagia (difficulty swallowing). |
| Referral Providers | Gastroenterologists, Oncologists, General Surgeons. |
| Placing Providers | Gastroenterologists (via endoscopy/ERCP), Interventional Radiologists. |
| Function | Provides internal drainage for bile or allows food/fluid to pass through a narrowed organ. |
| Permanence | Can be Temporary (plastic or partially covered metal) or Permanent (uncovered metal, for palliative care). |
| Types | Plastic Stents, Self-Expandable Metal Stents (SEMS) (covered or uncovered). |
4. Ureteral Stents (Genitourinary)
Used to keep the ureter (the tube connecting the kidney and bladder) open.
| Feature | Details |
| Symptoms/Conditions | Kidney stones (to relieve obstruction and swelling), Ureteral strictures, external compression from tumors. |
| Referral Providers | Emergency Physicians, Primary Care Physicians, Oncologists. |
| Placing Providers | Urologists, Interventional Radiologists. |
| Function | Maintains drainage from the kidney to the bladder, preventing kidney damage (hydronephrosis). |
| Permanence | Temporary. Most ureteral stents are plastic and must be removed or exchanged periodically (e.g., every 3-6 months) to prevent infection or encrustation. |
| Types | Double-J (pig-tail) stents, metal mesh stents (less common). |
🛑 Medical Malpractice Resulting in the Need for a Stent
A stent is often a necessary procedure that follows a delayed or wrong diagnosis of a severe vascular or obstructive disease. Malpractice may allow a condition to progress to a critical stage needing an urgent stent. Examples include:
- Failure to Diagnose and Treat Coronary Artery Disease (CAD): A primary care physician or non-invasive cardiologist fails to properly investigate and then treat escalating symptoms of angina or dismisses abnormal EKG/stress test results. The patient subsequently suffers a severe heart attack requiring emergency stenting.
- Misdiagnosis of Peripheral Artery Disease (PAD): A physician attributes symptoms of claudication or non-healing leg ulcers to a less serious condition (e.g., arthritis) and fails to order appropriate imaging (e.g., an ankle-brachial index or angiogram). The delay results in the progression of the arterial blockage, leading to critical limb ischemia and requiring urgent vascular stenting to prevent amputation.
- Negligent Management of Obstructive Jaundice: A patient presents with yellowing of the skin (jaundice), but the physician fails to promptly order necessary imaging or refer to a gastroenterologist, allowing a tumor or stone to completely obstruct the bile duct, requiring an emergency biliary stent.
In these cases, the negligence is the omission or delay that made the stenting procedure necessary to avert a catastrophic outcome.
⚠️ Medical Malpractice in Stent Placement and Management
Malpractice can also occur during or immediately following the procedure itself, often due to a violation of interventional protocol.
1. Technical Medical Malpractice During Stent Placement
- Wrong Site or Wrong Stent: Placing a stent in the wrong artery or organ, or using a stent of the wrong size, leading to immediate failure, migration, or rupture.
- Vessel Perforation: Negligently manipulating the guide wire or catheter, causing the artery wall to tear or rupture (perforation), leading to uncontrolled bleeding (tamponade in the heart or severe hemorrhage elsewhere). This is a known risk, but failure to recognize and immediately manage it (e.g., with a covered stent or emergency surgery) can constitute negligence.
- Embolization: The placement procedure dislodges a large piece of plaque or a clot (thrombus) that travels downstream and blocks a smaller, critical vessel (e.g., an artery supplying the brain or an extremity), causing a stroke or limb ischemia. While a risk of the procedure, failure to use clot prevention or protective devices where needed can be malpractice.
2. Post-Procedure Stent Medical Malpractice and Follow-Up
- Failure to Manage Antiplatelet Medication: After a coronary stent placement (especially a DES), the patient must take dual antiplatelet therapy (e.g., aspirin and clopidogrel) for a specific period to prevent the formation of a clot within the stent (stent thrombosis). If the placing physician or the treating physician negligently fails to prescribe these drugs, or inappropriately stops them early, and the patient suffers a severe stent thrombosis and a subsequent heart attack, this is a clear breach of the standard of care.
- Failure to Remove Temporary Stents: In the case of temporary ureteral or biliary stents, the physician has a duty to ensure the stent is removed or exchanged before it becomes calcified (encrusted) or causes a severe infection. Failure to schedule or communicate the follow-up procedure, then leading to an emergency, complex surgery for removal, may be malpractice.
In sum, the use of stents has improved medicine, but the complexity and gravity of the procedures mandate a high degree of skill. Deviations from the recognized standard of care at any stage—from the initial decision to stent to the post-procedural management—can result in devastating outcomes and subsequent legal liability.
If you have been injured in connection with a stent, contact the Kopec Law Firm.
Visit our free consultation page or video. Then contact the Kopec Law Firm at 800-604-0704 to speak directly with Attorney Mark Kopec. He is a top-rated Baltimore medical malpractice lawyer. The Kopec Law Firm is in Baltimore and pursues cases throughout Maryland and Washington, D.C.





