Mark Kopec Now
Macrosomia
Your Legal Rights in Cases of Birth Injury with Baltimore Macrosomia Lawyer Mark Kopec
The arrival of a new baby should be a joyous occasion. However, when a baby is significantly larger than average, it is a condition known as fetal macrosomia. This condition can present unique challenges during pregnancy, labor, and delivery. While many macrosomic babies are born healthy, the condition increases the risk of birth injuries to both mother and child. Healthcare providers must properly anticipate, monitor, or manage these risks. If not, it can potentially lead to devastating, preventable harm and may constitute medical malpractice. If your baby is injured, you may need Baltimore macrosomia lawyer Mark Kopec.
The Kopec Law Firm provides this webpage to provide comprehensive information about fetal macrosomia. This includes its diagnosis, management, and potential complications. It also discusses the circumstances under which improper medical care can lead to a birth injury medical malpractice claim.
What is Fetal Macrosomia?
Fetal macrosomia is from the Greek words “macro” (large) and “somia” (body). It refers to a newborn who is significantly larger than average for their gestational age. Macrosomia is generally when a baby weighs more than 8 pounds, 13 ounces (4,000 grams).
The prevalence of macrosomia varies but affects roughly 10% of all pregnancies. Certain factors can increase the likelihood of a baby developing macrosomia. Baltimore macrosomia lawyer Mark Kopec can evaluate the condition of your baby and advise you of your legal rights.
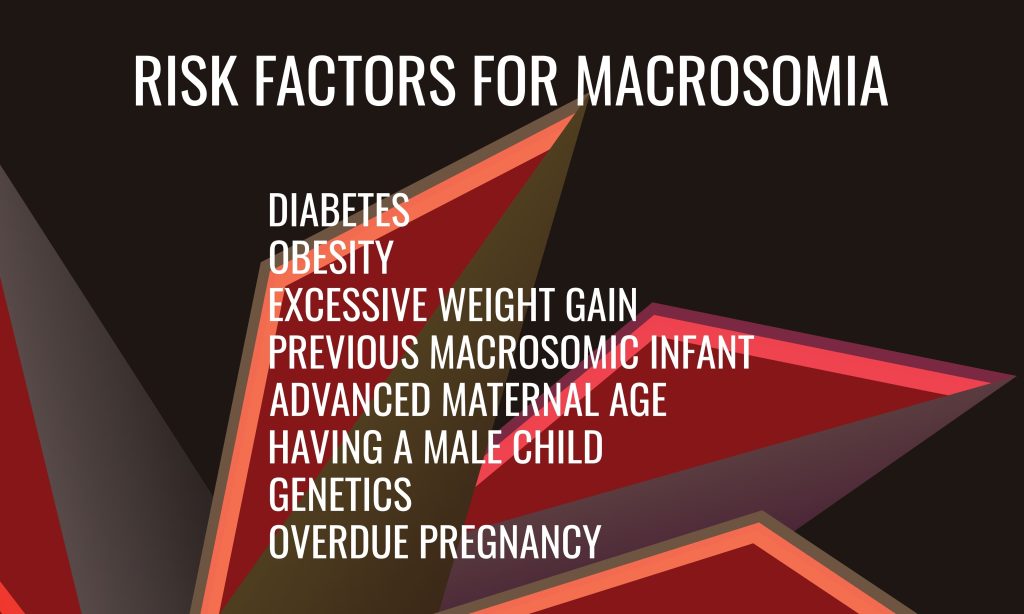
Key Risk Factors for Fetal Macrosomia
- Maternal Diabetes: This is one of the most significant risk factors. Pre-existing diabetes (Type 1 or Type 2) or gestational diabetes (diabetes that develops during pregnancy) can lead to higher maternal blood glucose levels. This excess glucose crosses the placenta. It causes the fetus to produce more insulin, a growth hormone, resulting in increased fetal growth and fat deposition.
- Maternal Obesity or High Body Mass Index (BMI): Women who are higher weight before pregnancy or who have a high BMI are more likely to have macrosomic infants.
- Excessive Weight Gain During Pregnancy: Gaining more than the recommended amount of weight during pregnancy can increase risk of fetal macrosomia.
- Previous Macrosomic Baby: A history of delivering a large baby increases the risk in subsequent pregnancies.
- Post-Term Pregnancy: Pregnancies that extend beyond 40 weeks (especially beyond 42 weeks) allow the fetus more time to grow.
- Maternal Age: Older mothers (typically over 35) may have a slightly increased risk.
- Male Fetus: Male infants, on average, tend to be larger than female infants.
- Genetic Factors and Maternal Birth Weight: A mother’s own birth weight and family history can play a role.
- Multiparity: Having had multiple previous pregnancies.
Baltimore macrosomia lawyer Mark Kopec will scrutinize the risk factors during your pregnancy.
Who Diagnoses Fetal Macrosomia and What Tests Are Used?
The diagnosis and management of suspected fetal macrosomia involves different doctors, primarily obstetricians (OB/GYNs). In high-risk pregnancies, a maternal-fetal medicine (MFM) specialist, an obstetrician with specialized training in managing complex pregnancies, may also assess the patient. After birth, pediatricians or neonatologists (pediatricians specializing in newborn care) will assess and care for the macrosomic infant.
Diagnosing macrosomia before birth can be challenging, and estimates of fetal weight are not always precise. Healthcare providers use several methods to assess fetal size during pregnancy:
- Fundal Height Measurement: This is a basic screening tool where the doctor measures the distance from the top of the mother’s pubic bone to the top of the uterus (the fundus). A fundal height that is significantly larger than expected for the gestational age can raise suspicion of macrosomia.
- Clinical Palpation (Leopold Maneuvers): Experienced clinicians can manually feel the mother’s abdomen to estimate the baby’s size and position. However, this method is subjective and less accurate, especially in higher weight women.
- Ultrasound: This is the most common imaging technique used to estimate fetal weight. Sonographers take various measurements of the fetus, such as head circumference (HC), biparietal diameter (BPD), abdominal circumference (AC), and femur length (FL). These measurements are then plugged into formulas to calculate an Estimated Fetal Weight (EFW).
Additional Tests
- Monitoring for Risk Factors: Regular prenatal care involves screening for and managing conditions like gestational diabetes and monitoring maternal weight gain, which are crucial in identifying pregnancies at higher risk for macrosomia.
- Antenatal Testing: If the doctor suspects macrosomia, particularly in conjunction with other conditions like maternal diabetes, they may perform tests such as nonstress tests (monitoring fetal heart rate in response to movement) or biophysical profiles (BPP) (ultrasound assessment of fetal well-being) to monitor the baby’s health.
Baltimore macrosomia lawyer Mark Kopec can assess whether the correct tests were used for your baby.
Potential Medical Responses and Management of Suspected Macrosomia
When healthcare providers suspect fetal macrosomia, they must engage in careful discussion with the expectant mother about the potential risks and benefits of various management strategies. The goal is to achieve the safest possible delivery for both mother and baby.
Potential Responses
- Management of Underlying Conditions:
- Diabetes Control: For mothers with pre-existing or gestational diabetes, strict glycemic control through diet, exercise, and medication (like insulin if needed) is paramount to potentially reduce excessive fetal growth.
- Weight Management: Counseling on appropriate weight gain during pregnancy.
- Delivery Planning and Counseling: This is a critical aspect of care. The obstetrician should discuss:
- Risks of Vaginal Delivery: Including prolonged labor, shoulder dystocia (see below), birth injuries to the baby, and increased risk of maternal trauma (e.g., severe perineal tears, postpartum hemorrhage).
- Risks and Benefits of Cesarean Delivery (C-section): The doctor may plan a C-section to avoid the complications of a difficult vaginal birth, particularly if the EFW is very high.
- Individualized Decision-Making: The decision should be individualized based on the EFW, maternal factors (pelvis size, previous delivery history), presence of diabetes, and the mother’s informed preferences.
- Induction of Labor (IOL):
- Historically, inducing labor earlier (e.g., at 39 weeks) was thought to potentially reduce the risk of macrosomia-related complications by delivering the baby at a smaller size.
Additional Responses
- Expectant Management with Close Monitoring:
- If vaginal delivery is planned, close monitoring of labor progress is essential. Healthcare providers must be prepared for potential complications like shoulder dystocia.
- This includes having experienced personnel available and a clear plan for managing obstetrical emergencies.
- Post-Delivery Care for the Newborn:
- Macrosomic infants are at higher risk for certain neonatal complications, such as hypoglycemia (low blood sugar), polycythemia (high red blood cell count leading to increased blood viscosity), hyperbilirubinemia (jaundice), and respiratory distress.
- These babies require careful monitoring and prompt treatment if these issues arise. They may also be at higher risk for childhood obesity and metabolic syndrome later in life.
Baltimore macrosomia lawyer Mark Kopec will examine the responses to your baby’s macrosomia to determine if they were insufficient.
What Can Happen if Macrosomia is Not Properly Responded To?
Failure to recognize the risks associated with macrosomia or to manage labor and delivery appropriately can lead to serious and sometimes permanent injuries for both the mother and the baby.
Potential Complications for the Mother
- Prolonged or Obstructed Labor: A large baby may have difficulty navigating the birth canal.
- Genital Tract Lacerations: Increased risk of severe tearing of the perineum (the area between the vagina and anus), vagina, and cervix. This can lead to third or fourth-degree tears, which involve the anal sphincter and rectum, causing long-term pain, incontinence, and sexual dysfunction.
- Postpartum Hemorrhage (PPH): A large baby can cause an overdistended uterus, leading to uterine atony (failure of the uterus to contract effectively after delivery), a major cause of severe bleeding.
- Uterine Rupture: While rare, this is a life-threatening emergency where the uterine wall tears. The risk is higher in women with a previous C-section scar (VBAC – Vaginal Birth After Cesarean).
- Need for Operative Vaginal Delivery: Increased likelihood of requiring forceps or vacuum extraction, which carry their own risks of trauma to both mother and baby.
- Emergency Cesarean Section: If labor fails to progress or fetal distress occurs, an emergency C-section may be necessary, which typically carries more risks than a planned C-section.
- Infection: Increased risk of chorioamnionitis (infection of the amniotic fluid and membranes) with prolonged labor.
Potential Complications and Birth Injuries for the Baby
- Shoulder Dystocia: This is one of the most serious complications. It occurs when, after the baby’s head has delivered, one or both shoulders become stuck behind the mother’s pubic bone, preventing delivery of the rest of the body. Shoulder dystocia requires specific maneuvers to free the shoulder.
- Consequences of Shoulder Dystocia:
- Brachial Plexus Injury (BPI): The brachial plexus is a network of nerves that runs from the neck down the arm, controlling movement and sensation in the shoulder, arm, and hand. A difficult delivery with shoulder dystocia can stretch, compress, or tear these nerves. This can result in conditions like Erb’s Palsy (affecting the upper arm) or Klumpke’s Palsy (affecting the lower arm and hand), leading to weakness, paralysis, or loss of sensation. Some injuries are temporary, but many can be permanent, requiring extensive therapy or surgery.
- Clavicle (Collarbone) or Humerus (Upper Arm Bone) Fractures: These can occur as a result of the difficult delivery or the maneuvers used to dislodge the shoulder.
- HIE: Hypoxic Ischemic Encephalopathy: If shoulder dystocia delays the delivery, the baby can lose oxygen, leading to brain damage. HIE can result in lifelong disabilities such as cerebral palsy, developmental delays, and seizure disorders.
- Fetal Death: In rare, severe cases, prolonged shoulder dystocia can be fatal.
- Consequences of Shoulder Dystocia:
- Birth Asphyxia/Hypoxia: Oxygen deprivation due to a prolonged or complicated delivery.
- Cephalohematoma: A collection of blood under the baby’s scalp.
- Facial Nerve Palsy: Due to pressure during delivery, sometimes from forceps.
- Neonatal Hypoglycemia: Low blood sugar shortly after birth, which, if severe or untreated, can cause brain injury.
- Respiratory Distress: Difficulty breathing, sometimes requiring respiratory support.
- Increased risk of Neonatal Intensive Care Unit (NICU) admission.
- Long-term health risks: Including childhood obesity and metabolic syndrome.
Types of Potential Medical Malpractice Claims with Baltimore Macrosomia Lawyer Mark Kopec
Medical malpractice occurs when a healthcare provider (doctor, nurse, midwife, or hospital) deviates from the accepted “standard of care,” and that deviation directly causes harm or injury to a patient. In the context of fetal macrosomia, several types of failures can lead to a medical malpractice claim if they result in a birth injury:
- Misdiagnosing, or Failing to Diagnose or Recognize Risk Factors for Macrosomia:
- Not taking an adequate maternal history (e.g., previous macrosomic baby, diabetes).
- Failing to screen for or appropriately manage gestational diabetes.
- Ignoring excessive maternal weight gain without proper counseling or investigation.
- Not performing or misinterpreting fundal height measurements or ultrasounds that suggest excessive fetal growth.
- Failure to Accurately Estimate Fetal Weight (within reasonable limits) or Appreciate the Significance of a High EFW:
- An underestimation or failure to consider macrosomia despite warning signs could be negligent.
- Failure to Counsel the Mother Adequately (Lack of Informed Consent):
- Not discussing the risks of macrosomia with the mother.
- Failing to explain the potential risks and benefits of vaginal delivery versus Cesarean section, especially when the EFW is in a range where C-section might be a safer option (e.g., >4,500g with diabetes, >5,000g without).
- Not allowing the mother to make an informed choice about her delivery method based on complete information.
Additional Claims
- Negligent Management of Labor and Delivery:
- Improper Management of Shoulder Dystocia: Failing to recognize shoulder dystocia promptly, using excessive or improper traction on the baby’s head and neck, not performing appropriate obstetric maneuvers correctly (e.g., McRoberts maneuver, suprapubic pressure, Woods’ screw maneuver), or panicking and deviating from established protocols.
- Inappropriate Use of Delivery Instruments: Negligent use of forceps or vacuum extractor, leading to trauma.
- Delay in Performing a Necessary Cesarean Section: Continuing to attempt a difficult vaginal delivery for too long and not doing a C-section for lack of progress, fetal distress, or intractable shoulder dystocia, leading to oxygen deprivation or other trauma.
- Failure to Have Appropriate Personnel or Equipment Available: Especially in high-risk deliveries where complications like shoulder dystocia are more foreseeable.
- Failure to Monitor the Fetus Adequately During Labor:
- Not recognizing signs of fetal distress on the fetal heart rate monitor that would warrant intervention, such as an expedited delivery or C-section.
- Failure to Resuscitate or Treat the Newborn Appropriately:
- Delays or errors in managing neonatal complications like hypoglycemia or respiratory distress that result in further injury.
If any of these failures occur and directly lead to a birth injury such as brachial plexus palsy, cerebral palsy due to HIE, significant maternal trauma, or other preventable harm, there may be grounds for a medical malpractice lawsuit. Such lawsuits seek compensation for the child’s medical expenses (past and future), pain and suffering, lost future earning capacity, and the costs of lifelong care and therapy if the injuries are permanent. Baltimore macrosomia lawyer Mark Kopec will explain all of these in more detail during your free consultation.
What to Do If You Suspect Medical Malpractice Related to Macrosomia
If your child suffered a birth injury and you believe the doctor mismanaged fetal macrosomia, it is crucial to:
- Seek Necessary Medical Care: Prioritize the health and well-being of your child and the mother.
- Document Everything: Keep detailed records of prenatal appointments, discussions with doctors, labor and delivery events, and all medical treatments.
- Request Medical Records: Obtain complete copies of all maternal and infant medical records from the hospital and all involved healthcare providers.
- Consult with an Experienced Birth Injury Attorney: We specialize in medical malpractice and birth injury cases. The Kopec Law Firm can review your records. We also will consult with medical expert witnesses. We will determine if the doctor breached the standard of care and if that breach caused the injuries. Then we can explain your legal options and guide you through the complex legal process. There are strict time limits (statutes of limitations) for filing medical malpractice claims, so seeking legal advice promptly is important.
Next Step: Call Baltimore Macrosomia Lawyer Mark Kopec
If you believe you or your child has been injured due to medical malpractice, it is important to consult with an experienced attorney to discuss your legal options.
Visit our free consultation page or video. Then contact the Kopec Law Firm at 800-604-0704 to speak directly with Attorney Mark Kopec. He is a top-rated Baltimore birth injury lawyer. The Kopec Law Firm is in Baltimore and pursues birth injury cases throughout Maryland and Washington, D.C.





